 A second case of the deadly MERS virus was recently confirmed in Orlando. It was found in a U.S. citizen returning from Saudi Arabia, where he was doing health work. He flew on multiple flights from Saudi Arabia to London, Boston, Atlanta, and then to Orlando.
A second case of the deadly MERS virus was recently confirmed in Orlando. It was found in a U.S. citizen returning from Saudi Arabia, where he was doing health work. He flew on multiple flights from Saudi Arabia to London, Boston, Atlanta, and then to Orlando.
Because of this, the Centers for Disease Control (CDC) is notifying passengers on his flights to be vigilant for symptoms, and to go straight to the doctor if anything surfaces. The patient is quarantined and in stable condition in the Dr. P. Phillips Hospital in Orlando, but a second case in the U.S. has many health officials concerned. Outbreaks of disease are on the rise, and not just the widely publicized MERS. Read on to see what’s happening and what you can do to keep yourself protected.
MERS
The biggest issue in the news has been Middle Eastern Respiratory Syndrome Coronavirus—MERS CoV, or simply MERS. There have been 538 confirmed cases since 2012—with 145 deaths—making it a 27 percent death rate.
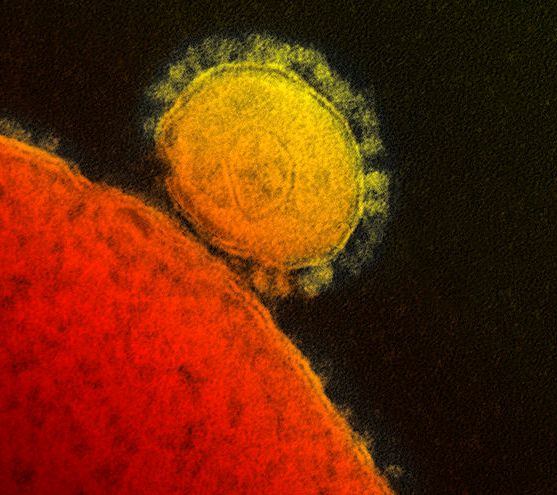 MERS is an upper-respiratory disease that affects breathing and produces flu symptoms, just like the SARS outbreak in 2003. Both MERS and SARS are in the family of coronavirus, but are distinct viruses. A coronavirus can infect both humans and animals.
MERS is an upper-respiratory disease that affects breathing and produces flu symptoms, just like the SARS outbreak in 2003. Both MERS and SARS are in the family of coronavirus, but are distinct viruses. A coronavirus can infect both humans and animals.
MERS seems to be less contagious than its relative SARS, but the reason for all the official worry and preventative effort is its deadlier 27 percent death rate, as opposed to SARS’ 9.6 percent. For comparison, cancer has an overall projected U.S. death rate of 35 percent for 2014 by the American Cancer Society.
The telltale symptoms of MERS are fever, cough, and shortness of breath, but can also include diarrhea, pneumonia, respiratory and kidney failure, and septic shock, according to the World Health Organization (WHO).
The majority of cases are in the Middle East. The concern is if the disease manifests in an area with limited healthcare resources, it would spread quickly, jumping to health officials, journalists, and other international workers who might bring it home on a plane.
The WHO reported a huge spike in April with over 250 cases. Every other month had less than 40 cases, and May has had the most cases of any month so far with over 50 and, unfortunately, counting.
There is no treatment or medicine for MERS. First reported in Saudi Arabia, it has since spread to the West and the US, with the first reported case in Indiana on May 2. It infects all ages and is assumed to have originated in camels.
Measles
A measles outbreak in the Philippines has been brought over by travelers to the US, with 129 reported cases. The Philippines has had over 20,000 cases of measles in only three months—January through March. The majority of the US measles cases has been in California, where parents can refuse vaccinations based on philosophical beliefs.
Measles was eradicated in the US in the 1950s, but every year a few cases are brought in with travelers. Due to the low level of cases and rising concerns over vaccinations, children can easily contract measles and go undiagnosed because doctors don’t have the personal experience to identify it.
Mumps
Mumps is having a resurgence on the eastern side of the US: 82 cases in Illinois, 328 cases in Ohio, and a couple dozen in New York and New Jersey. Most of these came from the universities of Ohio State, Fordham, and the Stevens Institute of Technology. The MMR vaccination is proven to be effective, but nothing can be 100 percent.
Mumps luckily is a self-limiting disease; it goes away on its own after a few weeks. However, it can sometimes cause dangerous inflammation in the brain and reproductive organs.
What to Do
With all of these communicable diseases, there is no specific treatment or medicine; the best idea is to see a doctor to check if it’s a serious case, then rest well and be as well fed as your body will let you.
For MERS, the CDC says you are not at risk if you have not had close contact with an infected person. It spreads through sustained contact, such as living with or caring for someone with the disease. If you’re in a high-risk area, the CDC recommends washing your hands often with soap and water (or if they’re unavailable, a hand sanitizer), being up to date with vaccinations, and avoiding touching the mucous membranes where the disease enters: eyes, nose, and mouth.
If you suspect you are sick, cover all sneezes with a tissue and throw the tissue in the trash, avoid contact with others, and see a doctor. Don’t be too alarmed if you feel sick, however. It could simply be the flu, because you would have to have been in direct contact with an infected person to contract MERS.
Measles and mumps are highly contagious. If there are people possibly infected around you, the CDC says the best thing to do is simply stay away for the first five days they show infection. Make sure your MMR vaccination is up to date. If you’re the one that’s ill, stay at home and away from people for at least five days.
For more information about staying healthy when you travel, check out:
- Why You Need Medical Travel Insurance
- A Closer Look at How Travelers Get Sick Overseas
- 4 Ways Your Hotel Can Make You Sick & How to Protect Yourself
- How You Can Avoid Norovirus On a Cruise
By Cody Brooks for PeterGreenberg.com